Dysregulated Behaviour Cluster
Home > TAND Clusters > Dysregulated Behaviour > What to seek
What to seek
The behaviours that have brought you to the dysregulated behaviour cluster include:
- temper tantrums (defined as an angry outburst, often in response to something that you or child did not want to happen),
- aggression (defined as behaviour that is intended to harm another individual), and
- self-injury (behaviour that is intended to harm you or the child themselves, such as hitting, biting, or scratching self).
These dysregulated behaviours can be common in children with TSC and can occur in adults as well. Strategies to deal with dysregulated behaviours may differ between children and adults. The impact of these behaviours on caregivers must not be overlooked or minimised. It is critically important for caregivers to care for themselves – please refer to the psychosocial cluster for support ideas and resources.
Understanding the meaning or function of behaviours
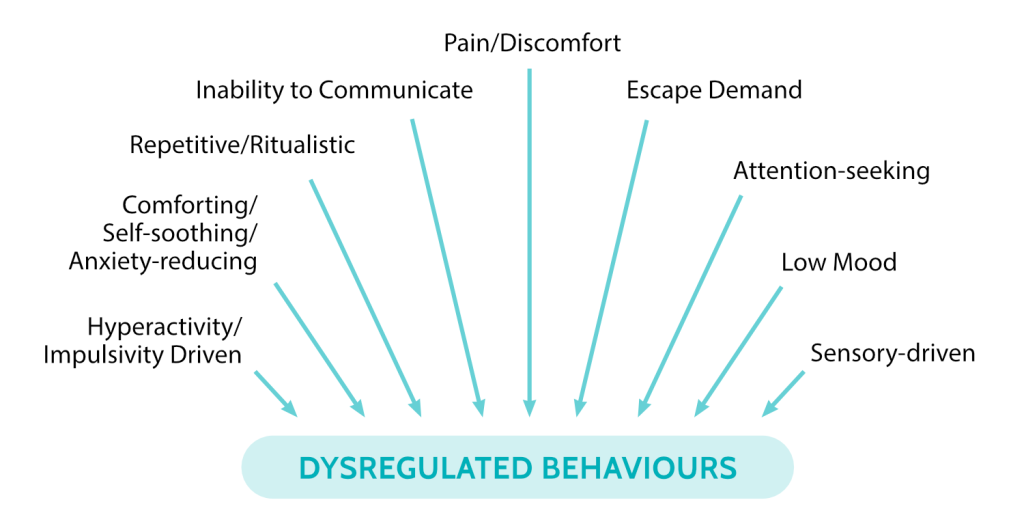
It is important to remember that all behaviour communicates! The chart below lists a whole range of reasons that an individual may display dysregulated behaviours:
The meaning of any dysregulated behaviour can be determined by tracking what happens before (antecedent) and after (consequence) the behaviour. Formally, this is known as a functional behavioural assessment (FBA).
We recommend that you seek help from a behavioural professional for a FBA to determine what may be underlying your or your child’s dysregulated behaviour. In some countries, this professional may be a board certified behavioural analyst (BCBA), whereas in other countries they may be a behavioural practitioner or specialist.
We recommend a medical evaluation if there is a sudden onset of behaviours, lethargy, signs of pain (see the FLACC pain scale in the eat/sleep cluster), or threat of serious injury to self or others. An evaluation should ideally be carried out by a medical practitioner in this case, along with other key members of your child’s medical team (for example, nephrologist or neurologist).
In the absence of a clear medical cause, consulting a behavioural psychologist can be very helpful in determining the reason for the dysregulated behaviour and coming up with a behavioural support plan together.
Applied Behavioural Analysis (ABA) therapy is based on the science of learning and behaviour. ABA therapy starts with the FBA, which provides data about the antecedents (what happens before the behaviour), the behaviour, and the consequence of the behaviour. The goal of the FBA is to identify the ‘function’ of the behaviour, e.g. a child who hits to escape the classroom. In this case, the function of the behaviour of hitting is escape. The next step is the drafting of a behaviour intervention plan (BIP). The behavioural therapist would draft a BIP to eliminate the behaviour of hitting in consideration of the child’s desire to escape, e.g. the child may be taught to ask for a break to encourage him or her to use words rather than hitting.
Learn more about Positive Behavioural support plans in the resource panel. You may also need to refer to the other clusters in this toolkit, for example the eat/sleep cluster, autism-like cluster, and neuropsychological cluster to determine if other developmental difficulties may be underlying behaviour.



